COVID vaccines: combining AstraZeneca and Pfizer may boost immunity – new study
Late last year, : is it safe to have more than one type of COVID-19 vaccine? A has now addressed that question, as well as what effect combining different vaccine types has on immunity.
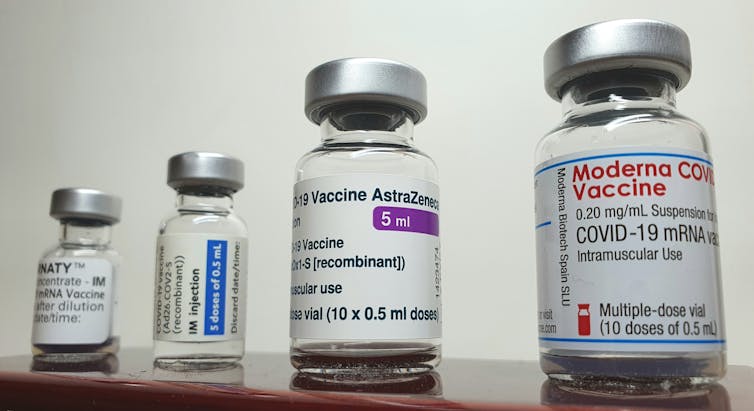
Most COVID-19 vaccines require two doses, and the usual strategy is to give people the same vaccine type for both. But the , led by the University of Oxford, recruited over 800 participants from across the UK to investigate the effects of giving people different vaccines for their first and second jabs. Two vaccines were studied: those made by Pfizer and AstraZeneca.
So, is mix and match an option? The are preliminary, having yet to be reviewed by other scientists, but the answer appears to be yes. Giving people different types of COVID-19 vaccine appears not only to be safe, but also a potential way of boosting protection against the coronavirus.
However, the exact benefits depend on which vaccine goes first and which second. Taking the AstraZeneca vaccine followed by the Pfizer one resulted in a striking increase in antibodies against the coronavirus’s spike protein (a key part of its outer structure) compared to using the AstraZeneca vaccine for both doses or Pfizer followed by AstraZeneca.
Taking the AstraZeneca vaccine followed by Pfizer resulted in a better T cell response than all other combinations of doses. T cells – also known as – are immune cells that help kill invading germs (such as the coronavirus) and support antibody production.
The Com-Cov study will next look at whether mixing and matching doses like this provides as good results when a larger gap is left between doses. The time between doses in this initial trial was 28 days, but a parallel study is stretching this to 84 days. The results are yet to be reported.
An expected outcome?
Other researchers have also been studying mixing vaccine types to fight COVID-19. A recently reported that people who initially received the AstraZeneca vaccine experienced a massive increase to their antiviral immunity when given a second dose of the Pfizer vaccine – providing more evidence that Pfizer works well as a booster.
 The body may mount an immune response against vaccines themselves – particularly those that use adenoviruses for delivery.
The body may mount an immune response against vaccines themselves – particularly those that use adenoviruses for delivery.
To understand why these beneficial effects might be happening, it’s important to understand how the AstraZeneca and Pfizer vaccines work. Both present a key element of the coronavirus – again, the – to the immune system, but do so using different methods.
The Pfizer approach packs the genetic code for the coronavirus’s spike protein into fatty nanoparticles. When these particles enter the body’s cells, the code is read and copies of the spike protein are produced, leading to an immune response. The AstraZeneca vaccine delivers the same genetic code but uses a weakened form of a common cold virus (an adenovirus) from chimpanzees to carry the code into cells.
When the first vaccine doses are given, it is possible that an immune response is raised not just against the spike protein created, but also against the carriers that are used to deliver the code for it. This is a for treatments or vaccines that use viruses for delivery. If the second dose is then the same, the immunity developed against the carrier will react against the second dose, clearing some of it before robust, protective and long-lasting immunity develops.
This is why Russia’s Sputnik V vaccine – which is based on the same delivery method as the AstraZeneca vaccine – uses two different adenoviruses as carriers for its first and second doses, and has achieved .
Why mixing doses is so important
There are additional benefits to mixing vaccine doses on top of improving protection. Logistical problems can arise when a second vaccine dose has to be identical to the first. Producing double the quantity of one vaccine takes time. Boosting with a different vaccine could allow the world’s population to be vaccinated quicker.
 Next we need to see what happens when mixing COVID-19 vaccines from other manufacturers.
Next we need to see what happens when mixing COVID-19 vaccines from other manufacturers.
Second, if a person reacts badly to their first vaccination, they are more likely to get a second dose if they know it is a different one – and it’s clear that for good protection. Governments may also decide a certain type of vaccine is less suitable for different groups of people, as with the AstraZeneca vaccine in younger people in some countries. Having more potential vaccine combinations available may help overcome any public uncertainty in the wake of these sorts of decisions.
Supplying vaccines to some low- and middle-income countries can also be difficult, particularly if they do not have the necessary cold storage requirements for large batches of a vaccine that need to be kept at low temperatures. Including vaccines into the distribution plan that do not need storage at very low temperatures may make widespread vaccine delivery easier.
So there are clearly huge benefits to vaccine mixing. However, this study only looked at two vaccine types – in time, every combination will need to be tested, in every age group and in every ethnicity. Vaccines may also behave differently if mixed in different contexts, for example, against a backdrop of malnutrition or other infectious diseases. These factors will need to be included in future testing too. But for now, this study suggests that a mix-and-match approach to COVID-19 vaccines is an acceptable, useful option.
, Professor of Inflammatory Disease,
This article is republished from under a Creative Commons license. Read the .